Systematic Digital dOCumentation and analysis of patient-reported outcomes (SysDOC)
Patient-Reported Outcome Measures (PROMs) are direct and unbiased data that patients provide regarding their perception of their health and disease status and their treatment. They are gaining increasing attention and importance with the goal of more patient-centered treatment. PROMs are relevant because not all aspects of a disease can be objectively measured and often would not be collected in a standardized manner without patient information. Especially in children, adolescents, and young adults, non-adherence is a complex factor that is influenced by multiple factors and is difficult to assess. Some of these factors are modifiable and can be monitored using PROMs. These include, for example, perceived health status, side effects of treatment, low health literacy, or psychosocial stress. The collection and analysis of PROMs could therefore significantly improve the early detection of non-adherence problems in the care of children with medical complexities (CMC).
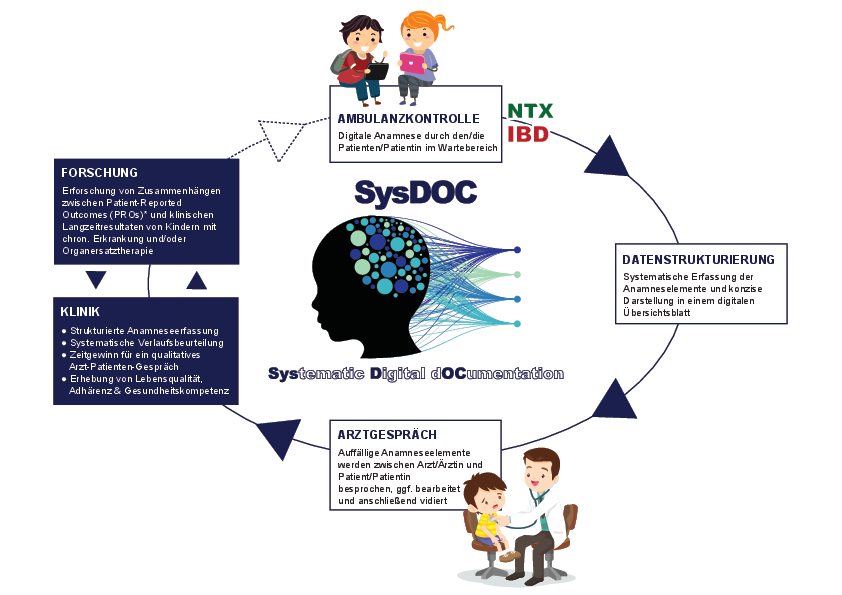
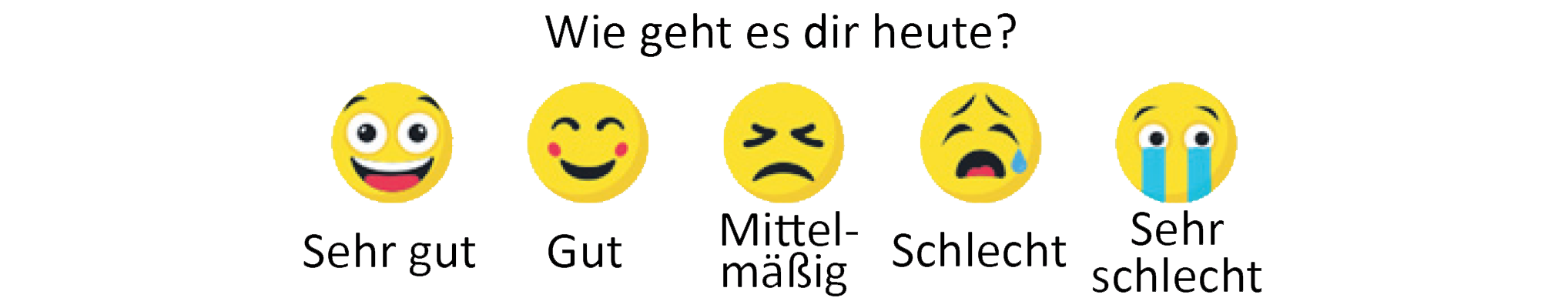
The focus is on the question of how PROMs can be collected digitally (ePROMs), and how these can then offer genuine clinical (scientifically evaluated!) added value for patients and their families, as well as for the interprofessional treatment team. This can be reflected in the early detection of disease changes, individualized therapy adaptation, or by strengthening participatory decision-making and education of patients and their families. A particular focus is on the practical design of the collection processes: How can ePROMs be integrated into routine documentation in a low-threshold, age-appropriate manner, and without additional burden? The goal is to develop a long-term, sustainable model that reflects both medical and psychosocial aspects of the disease.
Subproject 1:
Systematic Digital dOCumentation and analysis of patient-reported outcomes in pediatric kidney transplantation (Fabian Eibensteiner)
Approximately 5–10 children per million of the age-matched population suffer from chronic (end-stage) kidney failure, necessitating a kidney transplant in childhood. Due to the excellent short-term outcomes of kidney transplantation in childhood, research in this area focuses on long-term preservation of transplant function, management of complications due to the underlying disease and the required (immunosuppressive) therapy (e.g., infections, cardiovascular complications, post-transplant malignancies, adherence), general neurocognitive and pubertal development, and psychosocial aspects (e.g., quality of life, transition to adult medicine, education, and professional life). Nevertheless, in the long term, loss of transplant function is common (10-year transplant survival is 60–75%). One of the most common causes of loss of transplant function is lack of adherence to medication and therapeutic measures, which leads to subclinical rejection of the organ. Especially in children, adolescents, and young adults, non-adherence is a complex factor that is influenced by multiple factors and difficult to measure. Some of these factors are modifiable and can be monitored using PROMs (e.g., perceived health status, treatment side effects, low health literacy, psychosocial or family stress). The collection and analysis of PROMs could therefore significantly improve the early detection of non-adherence problems in the care of children after kidney transplantation.
Objectives of the project
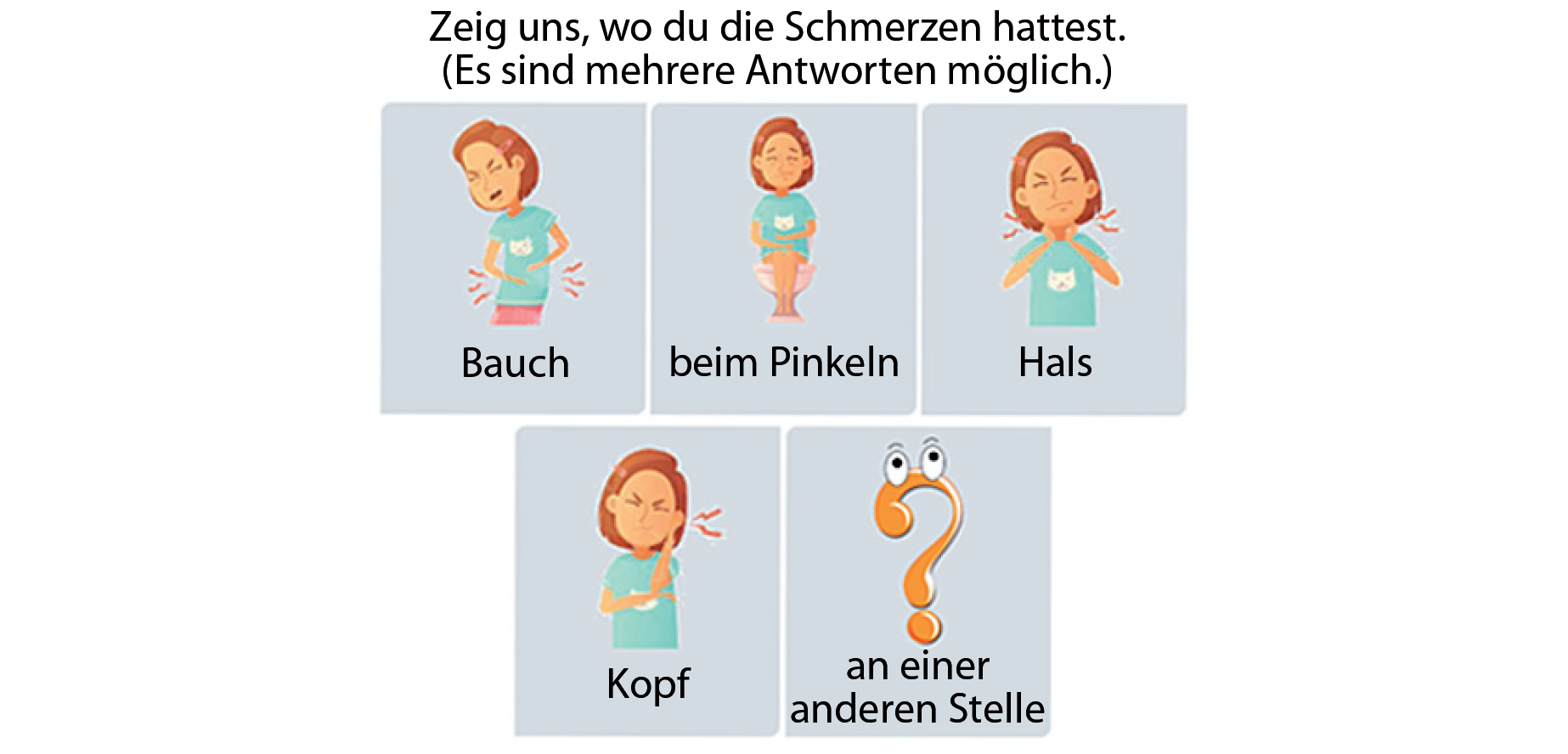
At each follow-up visit (every 4–8 weeks) in the outpatient clinic for pediatric kidney transplant recipients, a series of important medical history details, symptoms, and PROMs are collected using a tablet in the waiting area and restructured into a secure digital database. This was developed in an intensive process with the IT4Science team (led by Dr. Thomas Wrba) and the Outcomes Research team (led by Univ.-Prof. Dr. Tanja Stamm, project partner Valentin Ritschl, PhD). These data are correlated with clinical parameters of kidney transplant function and complications of kidney transplantation in order to identify patients at risk for loss of transplant function early and to intervene accordingly. In addition, patients will be phenotyped in detail using modern multi-omics technologies (e.g., plasma proteomics, metabolomics, and microbiome analyses of feces) in close collaboration with the Translational Laboratory of Pediatric Nephrology (Priv.-Doz. Dr. Rebecca Herzog) and the Core Facility Proteomics (Ap.Prof. Priv.-Doz. Dipl.-Ing. Dr. Klaus Kratochwill). The aim is to link biological patient phenotypes with symptom clusters and clinical outcome measures in order to develop hypotheses and explanations for possible causes of identified associations between symptom clusters and poorer transplant function. Furthermore, the barriers and facilitators for the introduction of such a digital medical history or ePROM collection tool into clinical routine will be identified and analyzed in a mixed-methods study (qualitative and quantitative data collection). The project is currently being expanded to include a systematic survey of fear of transplant loss (and thus progression of chronic kidney failure).
---------------------------------------------------------------------------------------------
Subproject 2:
SysDOC – Systematic Digital dOCumentation and analysis of patient-reported outcomes in pediatric inflammatory bowel disease (Rebecca Einspieler, Fabian Eibensteiner, Judith Hochrainer)
This subproject focuses on the use of ePROMs in children and adolescents with chronic inflammatory bowel disease, such as Crohn's disease or ulcerative colitis. ePROMs enable the continuous and structured digital assessment of symptoms (abdominal pain? dejection frequency? food intake?), quality of life, psychosocial stress, and limitations in daily life. A key component of this approach is the implementation and evaluation of these measures in the daily clinical practice of the pediatric gastroenterology outpatient clinic. These digital assessment tools open up new possibilities for a participatory, patient-educational, evidence-based, and structured longitudinal assessment of the disease and care, particularly for children and adolescents with chronic inflammatory bowel disease.
Subproject 3:
SysDOC – Systematic Digital dOCumentation and analysis of patient-reported outcomes in juvenile idiopathic arthritis (Isabella Valent, Fabian Eibensteiner)
Juvenile idiopathic arthritis (JIA) is a rheumatic disease that encompasses several subtypes and, depending on its severity, causes individual joint inflammations and associated pain, restricted mobility, or severe systemic inflammation. This project aims to investigate possible associations with clinical disease activity by using ePROMs representing various aspects of everyday life. Since the determination of disease activity in JIA has so far been primarily clinical – the laboratory parameters used are rather nonspecific – this study also utilizes newer analytical methods (proteomics, metabolomics, cytokine signatures) to analyze associations between specific PROMs and disease activity parameters.
Improving patient safety through structured communication
(Lisa Daniel-Fischer)
Discharge summaries serve as an important means of communication between healthcare providers, patients, and their parents. Although poor quality is associated with poor patient outcomes, the writing of discharge summaries is not taught in a standardized manner and is often left to the most inexperienced colleagues in everyday clinical practice. The aim of our project is to establish a hospital-wide training tool that will teach and facilitate the writing of discharge summaries for children and adolescents with chronic and complex diseases, while also improving the quality of discharge summaries. After conducting semi-structured interviews with pediatricians from tertiary and private practice settings, the first step was to create a checklist to support the writing and evaluation of discharge summaries. This checklist has been internationally validated by experts in the German-speaking countries, and its reliability has been tested within the hospital. A pilot study currently underway at the Department of Pediatrics and Adolescent Medicine and St. Josef Hospital Vienna will examine the impact of introducing this checklist into routine clinical practice on the quality of discharge summaries. Initial results are expected in fall 2025.
Patient safety in the area of high-risk medication
(Judith Hochrainer, Christoph Aufricht)
So-called high-risk medication is an essential component of drug therapy. While errors with this medication is not necessarily common, the consequences are often serious and can be associated with (life-threatening) complications. As part of our Animedes project, which is a follow-up to the findings of the publication by Selzer et al. (https://adc.bmj.com/content/109/3/215.long), we are investigating high-risk medication used for rheumatological, gastroenterological, and nephrological diseases. Our goal is to work with children and their guardians to find ways to avoid serious consequences from these particularly high-risk medication. In doing so, we aim to explore how safety and support in the use of this medication can be further improved in order to sustainably strengthen the health literacy, well-being, and quality of life of the affected children.
Subproject 1: Targeted Training for Subspecialist Care in Children With Medical Complexity (Fabian Eibensteiner, Rebecca Einspieler, Isabella Valent)
The aim of the project is to define particularly relevant training content in pediatric specialist training at a tertiary center using a needs assessment through a gap or discrepancy analysis. This analysis will determine the gap (= discrepancy) between the expected level of knowledge and skills and the actual subjectively experienced requirements in everyday clinical practice at the training unit. This needs assessment was conducted using a mixed-methods approach, including semi-structured qualitative interviews with residents from various pediatric disciplines at our clinic, followed by questionnaire surveys across the entire pediatric clinic. This was conducted in close collaboration with the Outcomes Research team (led by Univ.-Prof. Dr. Tanja Stamm, project partner Valentin Ritschl, PhD). Using a mixed-methods approach, the most important learning content for the training needs of future hospital physicians caring for children with medical complexities (CMC) was developed, emphasizing aspects of pediatric nephrology validated by an orthogonal method. A total of 280 listed topics within the content framework for pediatric residency training certified by the American Board of Pediatrics (ABP) were condensed into 23 important key topics in pediatric nephrology that require improvement through an Importance Performance Analysis (IPA) and validated in a larger cohort with regard to their importance for the training of future pediatric hospitalists. In particular, important aspects of patient safety beyond specialist training were highlighted, such as the principles of antimicrobial control and patient handover throughout the care chain, practical skills such as point-of-care sonography and blood product transfusions, and end-of-life care (palliative care). The knowledge base of this study forms the foundation for future detailed analyses and the development of digital bootcamps and could contribute to improving patient safety by reducing preventable harm from medical errors, particularly among vulnerable groups such as CMC in tertiary pediatrics. The study was published in the journal Frontiers in Pediatrics in 2022.
https://doi.org/10.3389/fped.2022.851033
Subproject 2: Evaluating essentials for Day One Competencies in Pediatric Rheumatology: A mixed-methods study (Isabella Valent, Fabian Eibensteiner, Judith Hochrainer)
Caring for children with rare diseases can be very challenging in a tertiary care center. Some patients are highly complex and are therefore cared for in specialized outpatient clinics. However, during initial consultations or in emergencies, care must be provided by colleagues who lack this specialized knowledge. This is particularly difficult in acute and potentially life-threatening situations. A training concept for pediatricians for the initial and emergency care of children with rare, chronic, and complex (rheumatological) diseases currently does not exist. This subproject aims to improve, establish, and re-evaluate training in the subfield of pediatric rheumatology using a targeted training approach.
Interviews with pediatric rheumatologists and pediatricians have created a knowledge base for the initial care of pediatric rheumatic patients. The qualitative, semi-structured approach allows theoretical knowledge to be linked with experience and emotions through free association, thus creating implicit knowledge. After transcription, condensation, and interpretation of the interviews, the meaning units are assigned to specific domains and evaluated and validated according to their importance in a Delphi process. The results of the study are intended to serve as a guide for pediatricians providing primary and emergency care to rheumatic patients during assessments or decision-making processes.
Long-term outcome after pediatric kidney transplantation: trigger tools and socioeconomic aspects (Lukas Kaltenegger)
This project focuses on data from patients who are cared for at the Division of Pediatric Nephrology and Gastroenterology, mostly before and especially after kidney transplantation. The information includes a detailed longitudinal breakdown of demographic and clinical facts – especially in the first year after transplantation. The analyses in this project concentrate on adverse events – events that lead to the need for unplanned outpatient or inpatient care after transplantation. The literature highlights the migration aspect of patients and their families as a relevant influencing factor, both with regard to access to medical care and the course of the disease. Investigating this parameter should help achieve optimal care for all affected patients in our patient population by enabling early identification of risk constellations.
M&M Conference (Isabella Valent)
Despite the best efforts of all involved, errors can occur in patient treatment. Morbidity and mortality conferences retrospectively review unusual treatment courses or (near-)complications experienced by patients. The goal is to improve patient safety and treatment quality by analyzing cognitive and systemic processes or structures for future patient care. Since errors often do not have a single cause, the M&M conference has several goals. It aims to promote systems thinking and metacognition, expand specialist knowledge, skills, and competencies, and, as a cultural representative, convey the values and attitudes of a department. Our department follows the principles of the Ottawa M&M Model and the guidelines for morbidity and mortality conferences of the Swiss Patient Safety Foundation (Stiftung Patientensicherheit Schweiz).
Early and integrative palliative care for children and adolescents with severe and life-shortening chronic illnesses (Christina Zachbauer, Christoph Aufricht, Martina Kronberger)
The Clinical Division of Pediatric Nephrology and Gastroenterology cares for children and adolescents with severe, complex, life-threatening or life-shortening chronic diseases of the kidney, liver, and gastrointestinal tract (Children with Medical Complexities, CMC-Children). These diseases are often associated with complex polysymptomatics, diverse psychological distress, and impaired quality of life for the patients, as well as with significant impacts on the entire family (parents, siblings, etc.). Conventional medical care by pediatric subspecialists (e.g., pediatric gastroenterologists, nephrologists) focuses primarily on treating organ-specific symptoms, while clinical follow-ups focus on collecting organ-centered biomedical information. The additional multiple problems and burdens associated with the holistic patient picture often receive insufficient attention in medical care.
Experts postulate that children with CMC and their families benefit from the early integration of a holistic, palliative care concept (CARE) into clinical care. Early integration of CARE leads to a significant reduction in symptom burden, improved quality of life, and promotes family-centered communication, shared decision-making, and active participation in life. However, our institution currently lacks adequate palliative care expertise and resources.
The MOMO4Care project aims to generate scientific evidence on the extent to which the clinical care of children and adolescents with complex, serious, life-threatening or life-shortening chronic illnesses can be improved long-term through early and integrative palliative care, thus making it available to all affected families. The project is a collaborative research project with the MOMO Children's Palliative Care Center, headed by Dr. Martina Kronberger-Vollnhofer.
https://www.kinderpalliativzentrum.at/de/
The hypotheses tested include whether a care intervention integrated early into specialized care has positive effects on the symptom burden and quality of life of children with CMC and underlying diseases of the kidney, liver, or gastrointestinal tract and their families. The intervention includes structured communication, standardized symptom management, and psychosocial support. Endpoints include the change in patient symptom burden from baseline to follow-up visits (assessed, among other things, with the PQ-MSAS) and the incidence of hospitalizations during the observation period.